Introduction
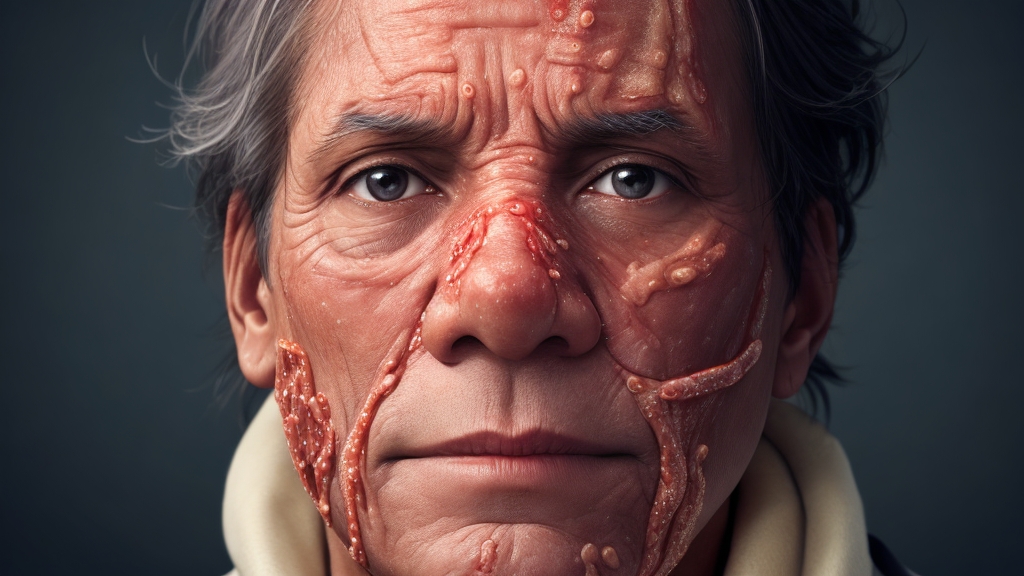
Skin ulcers, often overlooked and underestimated, are a significant medical condition that affects millions of people worldwide. These open sores on the skin’s surface can cause severe pain, disability, and, if left untreated, lead to life-threatening complications. In this article, we will explore the causes, types, risk factors, and available treatments for skin ulcers. By shedding light on this often-ignored condition, we hope to raise awareness and promote early intervention, thereby improving the quality of life for those affected.
Understanding Skin Ulcers
Skin ulcers, also known as pressure ulcers, bedsores, or decubitus ulcers, are localized wounds that result from prolonged pressure, friction, or shear forces on the skin. They typically develop over bony prominences such as the heels, ankles, hips, and tailbone. In these areas pressure and reduced blood flow can impair tissue health. However, bedsores can also occur in areas subjected to repeated trauma or with compromised circulation.
These wounds progress through several stages. Starting with mild inflammation, they progress to partial-thickness, loss of skin and eventually full-thickness tissue loss. In severe cases, ulcers can extend deep into the underlying muscles, tendons, or bones. This leads to serious complications like infections, cellulitis, or sepsis.
Types and Risk Factors
Skin ulcers can be classified into different categories based on their underlying causes:
- Pressure Ulcers: Result from prolonged pressure on the skin, commonly observed in bedridden individuals, wheelchair users, or those with limited mobility.
- Venous Ulcers: Caused by chronic venous insufficiency, leading to poor blood circulation and the subsequent breakdown of skin in the lower legs and ankles.
- Arterial Ulcers: Arise due to impaired blood flow, typically associated with peripheral artery disease, resulting in ulcers on the feet, toes, or lower leg.
- Diabetic Ulcers: Develop in individuals with diabetes due to nerve damage (neuropathy) and compromised blood supply, particularly in the feet.
Several factors increase the risk of developing skin ulcers, including advanced age, immobility, poor nutrition, reduced sensation, incontinence, chronic diseases (diabetes, cardiovascular disease), smoking, and obesity. Understanding these risk factors is crucial for preventive measures and early detection.
Treatment and Management
The management of decubitus ulcers requires a multidisciplinary approach involving healthcare professionals, including wound care specialists, nurses, and physicians. The primary goals of treatment include relieving pressure, promoting wound healing, controlling infection, and alleviating pain.
Treatment strategies may include:
- Pressure Relief: Frequent repositioning, the use of specialized support surfaces (mattresses, cushions), and regular movement to relieve pressure on affected areas.
- Wound Dressings: Appropriate dressings to maintain a moist wound environment, protect against infection, and facilitate healing. These may include hydrocolloids, foams, alginates, or antimicrobial dressings.
- Debridement: Removal of dead tissue or debris from the wound bed to stimulate healing. This can be achieved through various methods such as surgical, enzymatic, mechanical, or autolytic debridement.
- Infection Control: Administering antibiotics or antimicrobial dressings to prevent or treat infections. Close monitoring and regular assessments are essential for timely intervention.
- Nutrition and Hydration: Optimal wound healing requires adequate nutrition and hydration. A balanced diet rich in protein, vitamins, and minerals is recommended, along with sufficient fluid intake.
- Advanced Therapies: For complex or non-healing ulcers, advanced therapies such as negative pressure wound therapy, hyperbaric oxygen therapy, or bioengineered skin substitutes may be considered.

Prevention and Conclusion
Preventing skin ulcers is vital to reducing the burden of this condition. Some preventive measures include:
- Regular skin inspections: Check skin integrity daily, paying attention to areas prone to pressure or trauma.
- Proper positioning: Maintain good posture, use pressure-relieving aids, and avoid prolonged periods of immobility.
- Skin care: Keep the skin clean, moisturized, and protected from excessive moisture or dryness.
- Healthy lifestyle: Engage in regular physical activity, maintain a balanced diet, quit smoking, and manage underlying health conditions effectively.
- Education: Raise awareness among healthcare providers, caregivers, and patients themselves about the risk factors, early signs, and preventive measures for skin ulcers.
In conclusion, skin ulcers pose significant challenges to both patients and healthcare providers. By understanding the causes, types, risk factors, and available treatment options, we can work towards preventing, detecting, and managing skin ulcers more effectively. Early intervention, proper wound care, and a multidisciplinary approach are essential in reducing the morbidity associated with this condition. Let us strive to shed light on the hidden battle of skin ulcers and improve the lives of those affected by this often-neglected condition.